May 20, 2023
The Mother Who Changed: A Story of Dementia
The Mother Who Changed: A Story of Dementia by Katie Engelhart in the New York Times Magazine.
In October 2017, Diane Norelius stopped answering the phone. Her two daughters called and called. They called Diane’s boyfriend, Denzil Nelson, too. Whenever Denzil picked up, he would only say, “She doesn’t want to talk to you.” But usually, he didn’t pick up.
The women worried that their mother, who was 81, was sick, or maybe even dead. After a few days of radio silence, they flew home to Denison, Iowa, a town of around 8,000 people, surrounded by cornfields.
When Diane answered the door and saw her daughters standing on the lawn, she hesitated. Then she looked over at Denzil, who had come to stand by her side. “Can’t we come in, Mom?” Juli Norelius, her younger daughter, who is 59, remembers asking.
The farmhouse, once scrupulously tidy, looked unkempt. Inside the kitchen, the landline phone was missing, and the shelves were nearly bare. Only the freezer was full — and only with ice cream. On the stove, there was a piece of masking tape with Denzil’s handwriting on it: “DO NOT USE.” On a door frame, a large piece of wood blocked access to the staircase. Diane sat down at the round table, by the window.
Her curly white hair, usually puffed and set, lay flat around her neck. Her watch was on upside-down. She started speaking, but her words were slurred. After a while, Diane went to her bedroom and lay facedown on the bed.
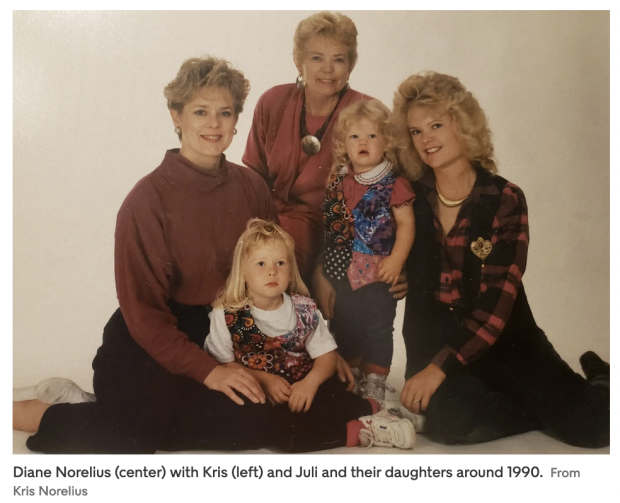
Kris Norelius, Diane’s older daughter, who is 65, had always considered her mother a very intelligent woman but also “very childlike.” Diane wanted to be taken care of — mostly by her husband, Bill. Throughout their decades of marriage, Bill gave Diane a weekly allowance, which she used to run the household. Otherwise, he took care of practical financial matters.
“I don’t know if I know the first thing about that sort of thing,” Diane later told her daughters. Diane raised money for the library and served on the local school board, but she always hurried home in time to fix Bill his lunch. Every afternoon, after school, she summoned her two daughters and her son, Erik, home with a large brass bell so that they could be standing at attention — faces washed, clothing presentable — when Bill arrived for supper.
When Bill died of complications from a broken hip in 2011, after 53 years of marriage, Diane found herself alone for the first time. Then, promptly, she lost more people. Juli, who lived next door, divorced and moved to Colorado: the last of the Norelius kids to leave town.
Then Erik died of cancer at age 55. Diane and Erik had always been especially close — when Erik was a boy, he used to vomit every morning before school because he didn’t want to leave his mama — and when he died in 2015, Diane started to unravel. In the midst of it all, she fell in love again.
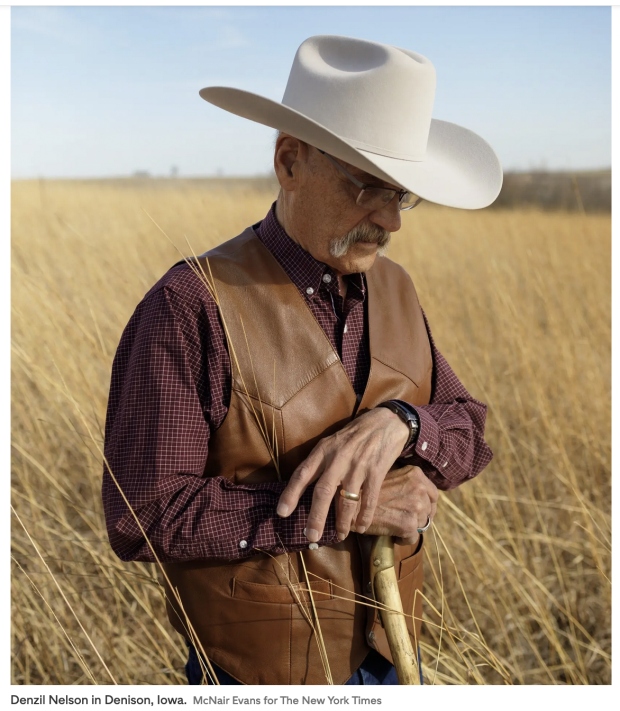
Kris took the news hardest. She lived in Oregon, with her husband, and decided to stop visiting Denison because she couldn’t bear to see “the paramour” in the house her dead father built. Juli, who owns a cattle business, just felt uneasy. Denzil, who is 84, was her ex-husband’s father: a man she was once close to but had distanced herself from after her bitter divorce.
The whole arrangement felt indecent and weird. For several years after Bill died, Denzil had managed upkeep on the Norelius farm: doing odd jobs and cutting the lawn with the big John Deere mower. But Diane had forever complained about him. She said he smelled bad.
She said that he stopped by for coffee sometimes and that she wished he wouldn’t. Now, as if all of a sudden, Denzil had moved in, and Diane was referring to him as “the love of my life.” To her daughters, it was grating — especially the way she said it quickly, as if it were all one word. Theloveofmylife!
Soon, she started dressing differently. Before, Diane had lived in colorful blouses from Chico’s and swinging pendant necklaces. Now she dressed like a cowboy, in stiff snap-button shirts tucked into bluejeans, even though she had never tucked her shirts into her pants because she thought it made her look fat.
he wore big leather belts too, and Denzil’s orange baseball cap. And sometimes the same outfit, day after day. She also looked much smaller. Kris and Juli knew that their mother had disordered ways of eating, but after Denzil moved in, she seemed to want to eat even less.
The sisters felt their joyous mother grow dour. She said mean things about dear friends. She stopped seeing them as much, and then not much at all. On the phone with Juli, Diane could be suspicious, even aggressive.
She wanted to know what was happening with her money. Juli would explain, again, what all of Diane’s assets were and how she was managing them safely, as Diane asked her to after Bill died.
But then, a few days later, Diane would call back with the same questions. Denzil had questions, too. Like: Why couldn’t Diane have more money in her checking account?
Juli started watching her mother’s financial transactions more closely. She knew that Diane — through her financial trust and her late husband’s trust, of which Diane was the sole beneficiary — was worth around $4 million. Denzil, a thrice-divorced retired horseshoer, was worth close to nothing.
It was only in September 2017 that a doctor in Denison finally gave form to what Diane’s daughters somehow knew and couldn’t see. Denzil had taken Diane to the emergency room because she felt short of breath.
There, she was given a cognitive test and scored poorly. She didn’t know the name of the president. She “definitely” had holes in her timeline, the doctor wrote. Diane was diagnosed with dementia.
Shortly after receiving her diagnosis, Diane rearranged her affairs.
She gave Denzil her financial power of attorney. Then, Denzil drove her to a lawyer’s office, where she redrafted her will, granting him the right to live in her “little house” — a small residence on her large property — when she died.
Around that time, Juli also found out that Diane had dissolved her financial trust, which held all her assets and investments and which Juli managed as trustee. When she checked Diane’s bank statements, she saw cash withdrawals of hundreds of dollars at a time.
Hours after Kris and Juli arrived at the farm that afternoon in October, two sheriff’s deputies pulled up. When the deputies entered the house, they carried a temporary protective order that the sisters’ lawyer had filed that day with the court. Under the terms of the order, Denzil would be immediately removed from Diane’s home and so “restrained from committing further acts of abuse or threats of elder abuse.”
The document contained a list of alleged offenses: coercing Diane into giving him access to her bank accounts; “deprivation of food, health care, supervision and hygiene.” Denzil “has virtually cut off all communication between Diane and her family,” the order read. “Diane has been diagnosed with dementia and does not have the ability to self-protect.”
Denzil stood motionless while the officers entered the house. Then he ran into the bedroom. In his telling, he leaned toward Diane and whispered, “Be tough, honey,” before collecting his various medications and his cowboy hat and driving away. In the sisters’ telling, he screamed at full hilt: “Look at what your [expletive] daughters are doing!”
“Where’s Denzil?” Diane asked her daughters after she woke up from her nap — and then again, all evening. And then in the middle of the night, and throughout the next day, too. Diane said that she and Denzil had plans to marry. She hoped he would make it back in time for the ceremony.
That day, Diane reached her hand toward the garbage disposal while it was running, and Juli leaped across the kitchen to pull it away before it was ground to bits. Later, she filled a washing machine with so much detergent that it overflowed. Kris had to carry armfuls of bubbles out the front door.
Kris and Juli decided that they would stay in Iowa, in the family home, until everything was sorted out. Kris would take a leave of absence from her job as an assistant to a financial adviser, and the sisters would apply to become their mother’s legal guardians. When family members called to ask how Diane was doing, it was hard to explain. Many metaphors of dementia describe total annihilation.
A person’s mind is ravaged or wrecked. A person’s essence is eroded or erased. Other common metaphors are thin and unserious. A person loses her marbles; loses her grip; loses the thread. She falls off her rocker. None of them worked. To her daughters, Diane was both familiar and totally strange.
For a while, the sisters wondered what their mother understood about her circumstance. Would she say the word “dementia”? Was she capable of scanning her internal landscape and seeing the advancing armies ahead? But Diane said nothing about it. As doctors would say later, she lacked “insight” into her condition.
All she did was say that she wanted Denzil. To Kris and Juli, it seemed their mother was too sick to even know what she wanted anymore.
Denzil said he fell in love with Diane in his truck. One day in 2012, he was doing odd jobs in the yard, and Diane asked what he was up to. He said he was about to go for a drive, and did she want to come?
“Well, where are you going?” she asked.
“I don’t know!” he said. That day, they took a short drive. After that, they took longer ones: to horse shows or quilt shows or antique sales. On their first two trips out of town, Diane and Denzil shared a motel room but slept in separate beds.
He stepped outside when she needed to change, and she did the same for him, because she was “a real lady.” But then one night, Diane climbed out of her bed and into his arms. Denzil thought Diane was the gentlest person he had ever known.
Sometimes, they would drive away from Denison without a plan — just straight out to nowhere. They drove to Montana and Arizona and all around the country. In the beginning, Diane was amazed to learn that Denzil never booked his motel rooms in advance:
He just drove until he didn’t feel like driving anymore, and then found a place to stay. “She thought that was the greatest,” Denzil told me. “She didn’t know you could go someplace without a reservation.” Bill had always made reservations. Diane later told her psychiatrist that Bill had been “very demanding,” but that Denzil wasn’t like that at all.
When Denzil moved in, Diane worried about what people in Denison would say. “Do you care?” Denzil asked, and Diane decided that she didn’t. They started holding hands when they went for walks along Main Street, and then for lunch at Cronk’s Cafe, a diner on an unlovely stretch of Lincoln Highway lined with auto shops and car dealerships. It was Denzil’s idea to eat in town every day.
“Diane had cooked all her life,” he told me. He thought she deserved a break. This, Denzil told his lawyer later, was why they did not have much food in the house when the girls stormed in.
The sisters weren’t happy about the relationship, but Denzil didn’t really care. Why should he? It seemed to him that Diane’s daughters were just interested in controlling things. Even Diane’s Social Security check went straight into an account managed by Juli.
Whenever Diane wanted to do anything — trade in her car for one she liked better, get rid of a messy tenant — Juli kicked up a fuss about how everything had to go through her because she was trustee of the Diane F. Norelius Trust.
Denzil said it bothered Diane that she couldn’t just do whatever she wanted, without having to explain herself or “beg for it.” He said Diane didn’t understand that it would be that way when she agreed to put Juli in charge of her finances.
Denzil was proud of Diane when she started standing up for herself on calls with Juli. He said he was encouraging her to be more assertive.
And the girls were forever nagging their mother to be careful. Don’t drive! Use a cane! Sometimes, Juli would call Denzil to say that someone in town had seen Diane walking around Walmart by herself, and why was she alone, and where was the cane? Denzil hated those calls.
What did they know about what Diane needed anyway? They didn’t live in Denison. Kris hadn’t visited in years. Denzil thought Diane’s daughters wanted Diane to be careful as if being careful was the most important thing in the world. Of course, Diane needed to be careful, but not only careful. She had to live too.
In the days after Denzil left the farmhouse, Kris, who wears her short gray hair swept to the right, and Juli, who wears her short blond hair swept to the left, sat down beside their mother. They told her, in as uncomplicated a way as they could, that Denzil had been abusing her. “That doesn’t mean that he hit you or anything,” Juli said. “We just need to figure out what’s going on.”
Sitting with her daughters, Diane could not quite remember appointing Denzil as her financial power of attorney. “What do you mean general power of attorney? What is a power of … ?” But she did remember revoking her financial trust. “And it has nothing to do with Denzil,” she said. “I want to be able to be my own person before I die.” Kris and Juli listened to their mother speak. But the Diane they knew had asked her daughters to take care of her.
In the philosophical literature on dementia, scholars speak of a contest between the “then-self” before the disease and the “now-self” after it: between how a person with dementia seems to want to live and how she previously said she would have wanted to live.
Many academic papers on the question begin in the same way: by telling the story of a woman named Margo, who was the subject of a 1991 article in The Journal of the American Medical Association (JAMA), by a physician named Andrew Firlik. Margo, according to the article, was 55 and had early-onset Alzheimer’s disease and couldn’t recognize anyone around her, but she was very happy.
She spent her days painting and listening to music. She read mystery novels too: often the same book day after day, the mystery remaining mysterious because she would forget it. “Despite her illness, or maybe somehow because of it,” Firlik wrote, “Margo is undeniably one of the happiest people I have known.”
A couple of years after the JAMA article was published, the philosopher and constitutional jurist Ronald Dworkin revisited the happy Margo in his 1993 book, “Life’s Dominion.” Imagine, he asked readers, that years ago, when she was fully competent, Margo had written a formal document explaining that if she ever developed Alzheimer’s disease, she should not be given lifesaving medical treatment.
“Or even that in that event she should be killed as soon and as painlessly as possible?” What was an ethical doctor to do? Should he kill now-Margo, even though she was happy, because then-Margo would have wanted to be dead?
In Dworkin’s view, it was then-Margo whose wishes deserved moral weight. In his book, he made a distinction between two kinds of interests: “experiential” and “critical.” An experiential interest was reactive and bodily: the pleasure of eating ice cream, say.
A critical interest was much more cerebral; it reflected the character of a person and how she wanted her life to be lived. In the case of advanced Alzheimer’s disease, Dworkin argued, there is a danger that critical interests will be usurped by experiential ones.
Still, it was the critical interests, previously stated, that deserved to be satisfied, because it was those interests that gave human life its meaning and its dignity — and even made it sacred, in a kind of secular way. A person was respected if she was helped to live out her chosen course, not if her life trajectory was allowed to be derailed by the amnesiac whims of her diseased self.
Some philosophers have devoted themselves to reconsidering Margo. They accuse Dworkin of holding too limited a view of meaning. Couldn’t a life of tiny pleasures be meaningful, even if it wasn’t the product of some sophisticated life plan?
Critics have asked why we should privilege the decisions of a person who effectively no longer exists over the expressed choices of the person who is sitting before us, here and now. On a practical level, what authority could the then-self possibly exert over the now-self?
And while Dworkin’s theory might apply to those in the advanced stages of the disease, it speaks less to a majority of patients in the mild and moderate phases. The in-between Margos. Dworkin’s theory also distinguishes between selves in a way that strikes some critics as misguided.
A person is not like Plutarch’s Ship of Theseus: replaced, plank by plank, over the course of her voyages, leaving those aboard to wonder if she is still the old ship or instead a new one — and, if she is a new one, when exactly she ceased to be the other. A person always is and is not who she used to be.
Still, many adult children cling to an image of a parent’s then-self and work relentlessly to protect it. Adult children “tend to be confident leaning on the side of a Dworkin-type view,” says Matilda Carter, a postdoctoral fellow in philosophy at the University of Glasgow and a former dementia caregiver.
They don’t want a parent’s confused, 11th-hour choices to “tarnish the legacy of her life beforehand.”
“I want to be my own person,” Diane told her daughters, again. “I want to be responsible.”
After the deputies came, Denzil moved into an apartment owned by his son Brad, because he had nowhere else to go. The apartment was above Brad’s law practice and a men’s clothing store called the Male Room.
Downstairs, in the office, Denzil sat with one of Brad’s colleagues and told him the whole story about “the sin sisters” and how they were trying to get control of their mother.
Peter Leo, a young associate lawyer, thought the temporary protective order against Denzil was a “total miscarriage of justice.” The judge, John D. Ackerman, had agreed to forcibly separate an older couple based on virtually nothing at all: just a few sentences written by Kris and Juli.
The sisters had claimed that Diane was sick and being abused and was “in need of immediate medical care.” But they hadn’t provided the court with medical records to prove it, and the judge hadn’t asked for them. He had not even bothered to speak to Diane. Under Iowa law, that wasn’t required.
Leo came to believe that Diane’s daughters had overreacted to a common diagnosis — and now were using the word “dementia” to maintain control over their mother’s estate. “The legal system is not set up to deal with this,” Leo told me. “As soon as you throw a loaded term like ‘dementia’ or ‘Alzheimer’s,’ everyone has a mental image of what that means.”
He added, “Your mind goes to a picture of a person lying comatose, drooling, whose mind has betrayed them.” A judge who hears the word “dementia” is liable to believe that the situation is an emergency if an adult daughter says it is.
In a letter to the court, Leo hypothesized that Kris and Juli’s elder-abuse petition “was filed in bad faith, and for the sole purpose of forcing a period of separation between Denzil and Diane.”
Denzil also seemed to have an explanation for everything. He insisted that he had been granted Diane’s power of attorney only because she had a tremor and worried that she might occasionally need him to sign checks on her behalf if her hands were shaking.
Denzil said the cash withdrawals from Diane’s bank account were for their trips out of town. He offered to turn over his bank and credit card statements to the court; he said he had nothing to hide. Denzil also said that he and Diane were planning to marry only because she wanted to. It was Diane who had proposed.
As for the house being unkempt, Denzil said he didn’t know what Kris and Juli were talking about. The house looked OK to him. Denzil didn’t like to see Diane on her hands and knees, scrubbing at the cabinets or the floor. Whenever she did, he told her to sit down and let him take care of it.
Besides, Denzil thought Diane was doing just fine. For years, he had taken her to her regular appointments with an advanced registered nurse practitioner; she knew more about Diane’s health than anyone, and she had never said anything about dementia.
At an appointment that spring, the nurse said that Diane’s cognitive tests were “normal,” though she thought her patient might have some “benign forgetfulness.”
Around Denison, people had started talking about what “the Norelius girls” were up to. Some people thought that Kris and Juli were after their mother’s money, as Denzil said they were. Other people said they were just big snobs — rich girls too good for Denison — who couldn’t stand to see their mother with a poor old horseshoer.
Diane’s friend Marcia Losh later told lawyers that she thought that Diane was being “held captive in her home.” (Losh declined to comment for this article.)
She said that when she went to visit Diane the day after Denzil’s banishment, Diane waited until her daughters’ backs were turned and then rolled her eyes in an exaggerated way — as if she needed to tell Losh something but couldn’t in front of her daughters.
Diane was entitled to her own lawyer to represent her in the elder-abuse proceedings against Denzil. Kris and Juli’s attorney, Maura Sailer, explained this to them — and at first, the sisters found it confusing, because how can a person with dementia instruct a lawyer all on her own? “Where do her rights begin and end?” Kris wanted to know.
Diane asked to meet with Denzil’s lawyer, Peter Leo, and Kris warily offered to drive her to his office. Kris expected the meeting to be brief. Leo was already representing Denzil in the elder-abuse case, and it wouldn’t make any sense for a single lawyer to represent both an accused perpetrator and his supposed victim. Kris waited for her mother in the reception area.
When Diane finally emerged from the office, Leo was standing at her side. “My client has something she wants to say,” he said.
“I have just learned what you girls have been up to,” Diane said. She didn’t seem angry, really, but she was very stern. She pointed at Kris. “I want you to go to the house, pack your things and leave.” In Leo’s office, Diane had signed an engagement letter, contracting the attorney to represent her.
‘Because she does not remember, she does not agree that she needs help.’
“Shame on you,” Kris said, pointing a finger at Leo. Then she reached for her mother’s arm.
Leo started shouting. “Take your hands off my client, or I’m going to call the police,” he said. In his office, Leo thought that Diane seemed “completely lucid” but also very frail.
She clearly did not want to leave with her daughter. Leo waited for Kris to drive away, and then he asked Diane where she wanted to go. She asked to stay with her friend Marcia Losh.
Within days, Kris and Juli filed a motion for immediate temporary guardianship and conservatorship of their mother, requesting full control of Diane’s personal care and finances. Under Iowa law, a person can be subject to guardianship if she has “decision-making capacity which is so impaired” that she can’t provide for her own safety and necessities.
The motion stated that it was in “Diane’s best interest” for her daughters to care for her, and that it was “not Diane’s true intent” for them to leave the family home. In a written statement, Juli acknowledged that her mother did not see things in the same way; “because she does not remember, she does not agree that she needs help.”
On Oct. 24, Judge Julie Schumacher granted Kris and Juli’s request and set a date in November for a hearing. In turn, Leo submitted motions to dissolve the protective order against Denzil and to suspend the temporary guardianship.
In a letter to the court, Leo wrote that Diane had the right “to vigorously contest her daughters’ claim that she lacks the decision-making capacity to manage her own personal and financial affairs.” Diane denied that Denzil had abused her in any of the ways her daughters said he did.
She said that Denzil made sure she ate “properly” and bathed “almost daily” and that he massaged her legs at night when they cramped.
Reluctantly, at their lawyer’s advice, the sisters agreed to drop the elder-abuse petition against Denzil and to focus on winning permanent guardianship of Diane. They also agreed to abandon their petition to be Diane’s conservators — and to recommend that a court-appointed banker or lawyer manage her accounts instead.
This, they hoped, would assure the judge that their claim to guardianship had nothing to do with Diane’s money. Kris left her job so that she would be ready to manage her mother’s care full time.
Denzil didn’t think that Diane needed a guardian, but if she had to have one, he said he wanted it to be him. He would fight the sisters in court. So would Losh, who said she worried about what Kris and Juli might do to their mother if they won. “We all know that Diane does have dementia,” Losh said later. “But the thing we need to do is care about Diane. She’s a person.”
In our own lives, we insist on the right to make our own choices, even bad ones — what is sometimes called “the right to folly.” As independent agents, we are free to be unreasonable and unwise and to act against our own best interests: maybe because of flawed reasoning, or just because we want to.
But with older relatives, we often insist on prudence over passion. “Ageism,” warns a 2016 paper in American Psychologist, “exacerbates the tendency to overprotect older adults.” In the end, this can mean that older people are held to a higher standard than everyone else; they are not allowed to choose poorly.
Any degree of cognitive impairment muddies these waters. When a person with dementia makes a decision that seems misguided, we might assume that the choice is not just bad but pathologically bad: a result of a cognitive failing. Eventually, each new decision — each expression of will — becomes suspect. Is this choice coming from Mom or from her disease?
If the former is true, the decision should be honored; if the latter is true, perhaps it should be thwarted. But as the disease progresses, this effort at cognitive sorting becomes less tenable, because how do you separate a person from her diseased brain anyway?
The more advanced a person’s dementia, the more her every choice becomes disputable, and thus worthy of custodial intervention.
“The question becomes, for the older adult, what are the barriers to evolving, to changing your opinions, to forming new relationships?” asks Nina Kohn, a law professor at Syracuse University with a specialty in the civil rights of older people. “When you form these new relationships, does that trigger people trying to remove your rights? The answer is: In some cases, it does.”
In particular, “decisions that seem atypical are going to be treated as suspect.” An older man who spent his life in a heterosexual marriage and now wishes to love another man might, for instance, be restrained from doing so. So might a woman who falls in love with a man decades her junior. Or, say, a wealthy 80-something widow who takes up with a horseshoer. “And all of those social biases are now being used to potentially undo individuals’ decisions while they’re still alive.”
Sign up for The New York Times Magazine Newsletter The best of The New York Times Magazine delivered to your inbox every week, including exclusive feature stories, photography, columns and more. Get it sent to your inbox.
Many adult children are surprised to learn that a diagnosis of dementia, on its own, does not disqualify a parent from making big decisions.
The adult child assumes that the first pronouncement from a doctor — that an older parent is cognitively impaired — immediately flips some kind of decisional switch, rendering the parent incompetent to choose.
Within medicine, there is no such switch. To an informed clinician, patients are never “capable” or “incapable” in a global sense. Instead, they are capable or incapable of making a specific decision, in a specific context, at a specific moment.
In practice, this means that a person with dementia might retain what doctors call “decision-making capacity” for years and then lose it in stages: the complex choices first, the simple ones later. She might, for instance, lose the capacity to choose among treatment options but retain the capacity to decide which family member should make the decision for her.
In each case, the firm bioethical consensus is that we should err on the side of assuming capacity. A person is capable until proved otherwise, even if she has dementia.
Standard cognitive tests, like the one administered to Diane in the local emergency room, can be useful pieces of evidence — a very low score would suggest, but not prove, that a person may be incapable of medical decision-making — but these tests are meant as screening tools and do not specifically measure decision-making ability.
As such, they offer little guidance to caregivers who are struggling to safeguard a loved one’s autonomy while protecting her from her compromised self: Where do we draw the line for a woman with dementia? How do we know when she has crossed it?
Until the early 20th century, things were less equivocal; a diagnosis of dementia, in and of itself, rendered a person medically “incapable” — as did other, now-antiquated diagnoses, like “lunatic” or “idiot.” It was only in the 1970s that capacity and medical diagnosis were delinked — in large part in response to the disability rights movement.
Physicians now rely on a framework for assessing capacity that was published in 1988 by the researchers Paul Appelbaum, a psychiatrist, and Thomas Grisso, a psychologist.
Under their terms, patients are capable of making medical choices if they can understand the relevant information; appreciate the nature of their condition as well as the risks and benefits of treatment; reason their way to a conclusion; and communicate their choice. Medical students across the United States now learn this in shorthand: understand, appreciate, reason, express a choice.
Still, the precise work of measuring self-sovereignty remains inexact. Decades after decision-making science took hold in American medicine, there is still no universally agreed-upon test of capacity — and no flawless gold standard by which to measure it.
Different doctors can come to different conclusions about the same patients, and they often do. A 2011 study published in Psychosomatics asked five psychiatrists to review 555 videotaped interviews with 188 people with Alzheimer’s disease; it found “considerable variability in capacity judgments.”
This variability is consequential, in part, because of the way it affects the course of lawsuits. Once, the law was as rigid as medicine; a diagnosis of dementia was itself enough for a judge to swiftly strip a person of her civil liberties and place her under the legal guardianship of another.
But in recent decades, the justice system has slowly moved in the direction of medicine, to recognize a more fluid notion of legal competency — sometimes with the help of doctors, who are brought into courtrooms to serve as expert witnesses, testifying to the particularities of their patients’ mental landscapes.
Within the legal world, “there has been, in the last several years, a real sea change in thinking about capacity,” Charlie Sabatino, former director of the American Bar Association’s Commission on Law and Aging, told me. “The real die-hard view is that you never lose capacity.”
In this newer view, a person can occupy an infinite number of spaces on a gradient from legally capable to incapable, with the far end of the spectrum reserved for people stuck in comas or vegetative states. Short of that extreme, a person will almost certainly retain the ability to choose some things for herself, even if she can’t choose everything.
A person might, for instance, be legally incapable of carrying out a complex property transaction but capable of managing a small bank account.
Today even a legal decision made in a fleeting moment of lucidity — a few minutes of clarity, pressed between hours or days of cognitive shadow — counts under the law. Even a decision that is later forgotten — like appointing a new power of attorney — counts.
Increasingly, conflicts about legal capacity are emerging in the context of estate planning. It is not uncommon for a person with early-stage dementia to write a new will or revise an old one — and then for an adult child to challenge the change in court.
The resulting lawsuit will hinge on whether the impaired parent had decision-making capacity at the moment she lifted the pen to sign her name.
Here, the legal system can stumble over medical uncertainty. Different doctors can come to different capacity judgments.
And legal challenges are often made weeks or months after a contract is signed, at which point a person with dementia will most likely have fallen deeper into her disease. In the end, in legal disputes about cognitive capacity, it is not doctors but judges and lawyers who have the final say.
What they needed, the sisters decided, was more evidence of what they already knew: that Diane was much sicker than she might initially seem.
They needed a full medical assessment. On Oct. 25, Kris and Juli drove their mother four hours east to the University of Iowa Hospitals & Clinics, where there was a dedicated geriatric-psychiatry unit.
Diane was examined by a dietitian, who found her to be mildly malnourished. She was also given a battery of blood tests and an ultrasound, during which a clinician noted that Diane did not have a gallbladder. Diane couldn’t remember what happened to it.
Physicians also reviewed Diane’s medication list and discontinued several: an anti-seizure medication that Diane did not know why she was taking, and lorazepam, which had been prescribed for anxiety.
This was routine. Dr. Judith Crossett, one of the unit’s geriatric psychiatrists at the time, often weaned older people off medications they didn’t really need: pills that were prescribed by many doctors over many years.
Older patients sometimes showed up at the hospital with literal bags of pills.
Next, Diane agreed to have a full neuropsychological exam. She told the examining psychologist that she had been married to her husband for 53 years.
Or was it that he died when he was 53? Maybe, she said, Bill died in 1953. In the end, the psychologist found that Diane had “significant deficits” in almost every field that he tested for and that she was unable to perform tasks as complex as meal preparation.
Because of this, she had “significantly limited capacity for informed personal, medical and financial decision making.” Diane was judged to be “attentive” and “expressive” but “insightless.”
She wanted to ask how a woman with Alzheimer’s disease was allowed to sign away thousands of dollars to a lawyer she had never met or spoken to, from a psychiatric unit.
In Crossett’s view, Diane was already in a “late moderate” stage of Alzheimer’s disease: far beyond the mild forgetfulness that her nurse practitioner in Denison observed.
The thing was, she said, “Diane talks well.” Many people with Alzheimer’s disease develop some form of aphasia, which affects their ability to understand language or self-express; these patients often use slow or halting speech or nonsense words, or they say “chair” when they mean “table.”
But Diane didn’t do that. She retained a “high level of social skills.” Later, Crossett explained that Diane “will fool most of the people, most of the time.” She went on, “She doesn’t look or sound like she has dementia to many people who don’t know what they are dealing with.”
What Crossett and her colleagues did not see was any evidence that Diane was a victim of elder abuse, as her daughters claimed. Doctors in the ward also balked when Kris asked them to ban visitors and restrict phone calls, and when she took Diane’s cellphone away, because, Kris said, Diane was in a fragile state and needed to rest.
A hospital social worker had to insist that Diane be able to speak with an attorney.
Juli went back to Denison, leaving Kris in Iowa City to be near Diane. At the farmhouse, she spent her days compiling timelines and collecting evidence of Denzil’s misdeeds and then writing out summaries of the evidence — until she had gathered so many documents that she started to forget where she had filed them all away.
“It was hard to focus, to keep track of things,” she said. She was tired. Juli also worked on finding her mother a new place to live. When Bill, in his later years, needed to go into a nursing home, Diane insisted that no facility in Denison was good enough for him and paid to move him into a more upscale place in Omaha.
he made her daughters promise that if she ever got sick herself, they would do the same. But when Kris showed Diane a brochure for a facility in Oregon, a few minutes from her own home, Diane wanted nothing to do with it. She wanted to stay in Denison.
Around that time, Peter Leo decided to withdraw his representation of Diane — in part to focus on other cases, he said — and drove to Iowa City to tell her that he had found her another attorney.
Sitting across from Leo, in a small meeting room, Diane signed a check for $3,000 to cover the new lawyer’s retainer fee. Kris stood in the room, her back pressed into the wall.
She was afraid to say anything that could be used against her later, but she wanted to ask how a woman with Alzheimer’s disease was allowed to sign away thousands of dollars to a lawyer she had never met or spoken to, from a psychiatric unit.
“The Ward loves her daughters very much,” Diane’s new lawyer, Alyssa Herbold, wrote in a petition to the court, “but asks that they let her be happy and allow her to reside in a facility in Denison, Iowa.”
“Who do you want to be your guardian?” Herbold had asked Diane.
“Who do I want to be my guardian?”
“Yes, the person who takes care of you.”
“Are you talking about taking care of me or taking care of something else?”
“Taking care of you.”
“Taking care of me? Denzil Nelson.”
In December 2017, Judge Schumacher ruled that Diane should stay in Denison until the guardianship trial, which was scheduled for the following spring.
In the meantime, Kris and Juli would remain as their mother’s temporary guardians, but the restraining order against Denzil would be dismissed, and he would be free to visit Diane every day between 7 a.m. and 7 p.m. — even if Diane’s guardians said he couldn’t.
Diane’s lawyer drove her straight from the courtroom to an assisted-living facility, Reed Place, which was named for Denison’s most famous resident, the actress Donna Reed.
It was located on a quiet street near Donna Reed Road, a few minutes northeast of the Donna Reed Theater. The judge had chosen the facility despite Juli’s protests that it was meant for older adults who were independent in “activities of daily living” and did not have a memory-care program or nurses with a specialty in dementia care.
At the facility, a nurse gave Diane a short cognitive test and a functional assessment; she judged that her patient’s cognition was “normal” and that Diane was “independent.” The nurse later said that she was never told by supervisors that Diane had a diagnosis of Alzheimer’s disease.
On her first night in her new room, Diane had a panic attack and called 911. Diane’s nurse practitioner wrote her another prescription for lorazepam, to be used during panic attacks, and one for the antidepressant Zoloft.
Still, Diane would sometimes cry in the night. 2 a.m., 3 a.m. “We’re having trouble,” someone at Reed Place would tell Denzil on the phone. “Can you come?” When he got there, Denzil would do his best to settle Diane. He would kiss her and tell her that it was going to be OK.
He would rub her legs if they were hurting. Sometimes that worked, but if it didn’t, then a nursing aide would come and give her what Denzil called a “stress pill.”
Denzil didn’t mind the interrupted nights because he woke early anyway. Most mornings, he was eating breakfast by 5. His clock had been set that way, from decades spent shoeing horses at sunrise. Either way, he would be at Reed Place at 7 a.m., so that he could sit with Diane while she ate her breakfast.
Then they often went for a walk around the building; he calculated that 10 times around the hallway was a mile, and sometimes they walked it twice. They watched TV: “Law & Order,” the news, old westerns. They played cards. Diane might nap in the morning or in the afternoon.
She might get dressed in a paisley-patterned blouse, buttoned all the way up to her neck, so that they could go to Walmart or eat lunch at Cronk’s.
In the evenings, Denzil and Diane would have dinner together, and Denzil would leave just before 7 p.m., his court-mandated departure time. “TOUGH TIME SAYING GOODNIGHT,” he wrote in his diary.
“REALLY HARD TIME SAYING GOOD NIGHT!”
“SAYING GOODNIGHT IS NOT GETTING ANY EASIER.”
“WORST GOOD NIGHT EVER.”
Denzil didn’t want to see Diane’s daughters, and Diane said she didn’t want to see them either — and the nurses at Reed Place said she didn’t have to.
On one of his first visits to the facility, Denzil unplugged the landline phone in Diane’s room, and he bought her a new cellphone without giving Kris and Juli the number. When Kris and Juli called the front desk, their calls were not put through.
“My client does not want to see her daughters for Christmas or the foreseeable future,” Herbold wrote in an email to their lawyer. (Herbold declined to comment for this article.)
The sisters cried, but then they dropped off a card and a basket of gifts anyway. They tried to remind themselves that none of this was really coming from their mother; this was just the way of her disease.
Over the holidays, Kris and Juli thought a lot about the hours that Diane spent alone, with Denzil, in her new bedroom. The sisters assumed that their mother and Denzil were having sex — and that, if they were, it wasn’t sex at all but instead rape, because Diane was too impaired to consent to it.
In her reading, Kris learned that sex is one of the least studied and least discussed fields in dementia care. There are no validated clinical tools to specifically assess capacity for sexual consent, or even consensus guidelines. There is also no uniform legal standard.
Juli’s daughter, Hayley, who is 32, told her mother that she would visit Diane herself. From the start of the fallout, Hayley had tried to be impartial — or at least to seem that way — because of the strange position she was in; Diane was her biological grandmother, and Denzil was her biological grandfather, and she loved them both.
To Hayley, Denzil may have been an imperfect caregiver, but he was also a grumpy old man who didn’t necessarily know how to do things any better. And Hayley thought her grandmother benefited from the arrangement, too; Diane had someone to take her on adventures.
On the phone, in late December, Hayley asked Diane if she could come to visit, and Diane told her she could. But a few minutes later, Hayley said, Diane called back and said that Hayley couldn’t come after all, because she and Denzil were going to a party.
Hayley told me that she could hear Denzil in the background, coaching Diane on what to say (Denzil denies that he ever coached Diane).
The next day, Hayley got in her car and drove to Reed Place. She brought a little stuffed dog to give to her grandmother, because Diane had always liked that kind of thing. In the lobby, Hayley saw Denzil and Diane, and she met her grandfather’s eyes.
Then, she said, Denzil grabbed Diane’s elbow and started pulling her away. Hayley called out to her grandmother and ran toward her. Diane continued walking with Denzil, but also reached her arm out, behind her back, toward Hayley. “That’s my Nana,” Hayley told me. “She’s a people pleaser, and I know that she loved Denzil, and I know that she loved me.”
Hayley reached forward and put the stuffed dog in her grandmother’s hand.
“Drop it, Diane,” she heard Denzil say. And so Diane dropped it, and the two of them walked away.
Denzil thought that if he could keep Diane’s stress under control, she might get better — at least “somewhat.” That meant keeping certain people away from her: mostly Diane’s daughters, but also Hayley, who, he insisted, had “ambushed” Diane in the lobby, even though Diane told her not to come. Diane was so rattled after Hayley left that she had to take another “stress pill.”
At Reed Place, the stories that Diane told about her daughters grew more fantastical. She said that Juli had thrown her in the trunk of a car. She said that Kris had dumped her at the emergency-room door in Iowa City and then never came to visit.
The memories were false, but they didn’t feel that way to Diane. Alone with Denzil, her rage seemed to metastasize. “I have decided that I no longer have any daughters,” Diane said.
Depositions began in February, and the hearings ran into March. Each day in court, Diane sat beside Denzil. Her daughters observed that she wore the same shirt days in a row and would sometimes fall asleep during testimony.
Crossett, Diane’s psychiatrist from Iowa City, was called to testify about Diane’s diagnosis of Alzheimer’s disease. In her view, Diane lacked “the capacity to make safe choices for her finances, for where and how she lives.”
“Does Diane have the ability to make her preferences known?” Sailer, the sisters’ lawyer, asked.
“She certainly has the ability to say what she prefers,” Crossett said. “The analogy would be: My 6-year-old grandson states a great many preferences, but we allow very few of them to be carried out.”
Sailer repeated the doctor’s message to the court. “Although Diane retains the ability to express her preferences, her disease has taken away her ability to reason.” Diane could say what she wanted, but that didn’t mean that she really wanted it — or that she understood all the information that should reasonably have factored into her wanting.
And yet, there was Diane, proclaiming over and over what she wanted: for Kris and Juli not to be her guardians. What was the court to do with that? Diane’s lawyer urged the judge to honor Diane’s preferences, rather than allow them to be steamrollered by daughters who claimed to know better for her. “She wants to be included in things going on in her life.”
“My mother had a diagnosis of dementia,” Kris said, nervously, when Diane’s lawyer rose to question her.
“So do you believe that we shouldn’t listen to anything that your mother has to say because she’s been diagnosed with dementia?”
“I didn’t say that, but …”
In May, the judge issued her ruling. Diane would be placed under a full, or “plenary,” guardianship, as Kris and Juli had requested. But Kris and Juli would not be their mother’s guardians.
The judge noted that Iowa gives preference to in-state guardians, but she also voiced concern about the sisters’ “failure to give consideration to Diane’s wishes.” Denzil, too, would not be granted guardianship, in part because he seemed to have “an underappreciation of Diane’s dementia.”
This left Diane’s friend Marcia Losh as her new guardian.
Denzil thought that if he could keep Diane’s stress under control, she might get better — at least ‘somewhat.’ That meant keeping certain people away from her.
Instead of choosing between conservators, Judge Schumacher appointed two: a lawyer Kris and Juli had put forward and a retired judge named Edward Jacobson, whom Diane’s lawyer supported and who was, at the time, under a formal ethics investigation by the Iowa Judicial Branch.
(It was found that some of Jacobson’s legal decisions had been ghostwritten by attorneys involved in the cases.) The two men would each draw a salary of around $200 an hour from Diane’s estate.
Within hours of reading that they had lost the guardianship case, Kris and Juli were in a car on their way out of Denison. Juli was enraged. Over the next few days, she spent long hours working on an appeal. Kris didn’t feel angry because she couldn’t really feel anything.
Her daughter, Elise, felt her mother withdraw. For months, Kris had been subsumed by the fight over Diane — and the confusion and the injustice, until it was all she could think about and all she could talk about, the same thing over and over, without any sense of her own ceaselessness. Now she barely talked at all.
After the appeal came more lawsuits. Jacobson, the conservator, sued Juli, claiming that she had disparaged him and caused him financial distress.
Juli submitted a petition against both conservators. Jacobson and Losh, acting on behalf of Diane, sued Juli, accusing her of “looting” from her father’s trust, because Juli had used trust money to reimburse herself for expenses incurred while fighting for the guardianship.
The sisters filed a petition to remove Losh as guardian. Then Losh filed for a protective order against Juli after she posted about the guardianship battle on Facebook.
At some point, in the late summer of 2018, Juli heard a rumor that Diane and Denzil had been married, and she took Losh to court again — demanding that, as guardian, Losh seek an annulment, because the judge in the guardianship case had already ruled that Diane was too impaired to consent to marriage. (The marriage was annulled that November.)
This was all expensive. In the spring of 2019, the court ordered for over $130,000 to be paid out to lawyers. Then attorneys requested over $50,000 more. Jacobson hired his own lawyer to represent him in his case against Juli, and those legal fees were also covered by the trust: around $22,000.
There were now eight lawyers involved in the fight over Diane, nearly all being paid by her. Losh, who initially agreed to serve as guardian without pay, also asked the court for permission to start charging $40 an hour.
She was approved. Soon she was charging for the time she spent bringing Diane a cake ($40), sewing a tear in Diane’s shirt ($50) and speaking to Diane on the phone when she was confused ($20).
“Mom does not have the ability to understand that Marcia is billing every time she calls her for any reason,” Kris wrote in a letter presented to the court.
When Kris and Juli asked to meet with their mother, or even just speak to her, Losh said that Diane didn’t want to and that she wasn’t going to force her. “The chances of reuniting with your mother are extremely slim,” Losh told them.
Denzil, for his part, felt liberated. With Losh’s permission, he moved back into Diane’s house. He started arriving early at Reed Place and staying late. In the mornings, now, Diane had trouble putting on her makeup, so Denzil would do it for her. “I probably didn’t do a real good job,” he said. But “it was important to her.”
Diane told Denzil that when she died, she didn’t want to be buried in the Norelius plot, beside Bill. She wanted to stay with him. Denzil said OK, even though he knew this was a promise he probably couldn’t keep.
Now that the sisters were gone, Denzil and Diane could spend time at the house again. On many days, Denzil drove Diane back, up Highway 39, and the two of them would sit on the porch swing for hours.
Sometimes, he would get Diane in the car and drive right up to the property that Juli still owned next door, and Diane would raise her middle fingers at the security cameras: first one, then the other, her face impassive and unmoving.
In October 2019, Diane fell. She was in her room alone, in the evening, and lost her balance walking from the bed to the bathroom. The next day, she said her head hurt on one side; then she said it hurt on the other. She couldn’t point to exactly where the pain was.
The staff at Reed Place gave her Tylenol, but a few days later, Diane started crying and wouldn’t stop. Losh took her to the hospital. There, a doctor recommended that Diane be moved out of Reed Place and into a local nursing home called Eventide, which would help with daily activities like bathing and eating.
Losh agreed, even though Kris and Juli insisted that their mother feared Eventide more than any other place — and particularly, the cluster of basement rooms that housed dementia patients and was known as Memory Lane.
“Diane’s dementia has accelerated during this period,” Losh wrote in December 2019, in the annual report that guardians in Iowa are required to file with local courts. Losh said that Diane was feeling physically better, but that some days she “doesn’t know up or down, night or day.”
Kris and Juli didn’t understand how a woman who didn’t know up from down could remember to hate her own daughters, unless someone was reminding her to.
“What mother wants to get old without their family around them?” Kris asked me, tearfully.
When Covid hit, Eventide locked down, as did nearly every other nursing home in the country. Denzil still visited every day, because he thought it was important for Diane to see his face. If it was a warm day, he would sit outside her window. If it was cold, he would come inside, into a lobby area where he could look at Diane through a thick glass door and speak to her on the cellphone.
Diane would ask about his day, and he would ask about hers. But often, Diane couldn’t hear what Denzil was saying because of the way her hearing aids pressed against the phone. By summertime, Diane would forget that she was holding the phone and let it drop by her side.
Diane seemed to understand some things about the pandemic but not other things. She accused Denzil of choosing not to come inside to see her. “I know you can come here,” she would yell into the phone.
“You just don’t want to see me.” Denzil would explain the situation, but then she would forget again. He started visiting less, and then he didn’t visit at all. “I was not in very good shape at that time,” he told me, “but I did the best I could.”
From Colorado, Juli would occasionally ask friends to call Eventide and ask for Diane. Almost always, their calls were turned away, but in July, a woman named Mary was put through.
“Hi, Diane, how are you doing?” Mary asked, when Diane picked up.
“Well, I am not doing too fine right now. I have kind of lost myself,” Diane said. “I am in serious trouble because I don’t have enough money to get me out of here.”
“Diane, I am going to call your daughter Juli and ask her to help you. Can I do that?”
“Yes, you can.”
“She loves you very much, and she wants to come and see you.”
“Well, if you’d call her, I would appreciate it!”
A few days later, Mary called back. “So I called your daughter Juli, and she is finding a different place for you to live.”
“Oh, really?”
“Yes.”
“Oh, my goodness! So what do I have to do?”
“You don’t have to do anything.”
“Oh, that sounds absolutely wonderful,” Diane said, her voice shaking a little. “Oh, thank you.” Then she started to cry.
“No, don’t cry!” Mary said.
“It’s a happy cry,” Diane said.
Mary told Diane that Kris and Juli wanted to come see her. “Is that OK?”
“Yes. Absolutely. Thank you, sweetheart.”
At the end of the call, Diane forgot to hang up the phone. Mary stayed on the line to listen. Diane cried some more, and then she sat in silence. When a nurse came in to ask if she was OK, Diane sounded different. “They hate me,” she said.
“They hate you?”
“They call me bad things.”
After some time, Diane’s conservators insisted on selling her house and the objects inside, and Juli agreed to buy it all. She paid $200 for a clock that had been in the family for generations and $10 for a music box made by her father. She also bought back her own wedding dress.
By Juli’s calculations, the legal fight over her mother had by then cost over $400,000 in lawyer fees alone.
Without a place to live, Denzil filed for bankruptcy and moved into a small apartment, in a redbrick complex on a residential street. In his bankruptcy filings, Denzil calculated his total worth to be just over $21,000.
Asked to detail any “collectibles of value,” he had made note of a wooden rocking chair, a cast-iron lawn ornament and a “picture of Diane.”
In August 2020, Alyssa Herbold went to visit her client at Eventide’s courtyard entrance. Diane did not know her lawyer. She did not know how many children she had.
The following month, a court agreed with the sisters’ request that Diane be moved to Prairie Meadows, a specialized dementia-care facility in Omaha that Juli had found. By the time she got there, Diane was dying and was placed on hospice care.
It was around then that a judge finally signed an order granting Kris and Juli the right to see their mother for the first time in more than two years — regardless of Losh’s opposition.
Kris, who is immunocompromised, decided that it wasn’t safe for her to travel, but Juli got in her truck and drove nine hours to Nebraska. She spent four days with her mother: most of it in Diane’s room, talking about whatever, “nonsense stuff.” Juli wasn’t sure whether Diane knew exactly who she was, but she seemed to love Juli and want to be close to her.
The two women lay in bed together, propped up on pillows: Diane, stroking the stuffed toy dog that Juli had brought for her — the one that Hayley had tried to put in her grandmother’s hand. Diane said the dog liked to have its tummy scratched.
“Where’s … that man?” Diane sometimes asked.
Away from Denison, Kris and Juli had sometimes wondered about their mother’s inner life — and whether she had one anymore. It was hard to know whether a person who had lost so many autobiographical details to the advanced stages of the disease could still constitute her own self.
Many caregivers are convinced of the existence of an inner life, however buried away; they hope and pray that Mom is in there, somewhere. Others are horrified by the thought of their loved one’s living, somehow intact, inside a diseased mind.
Lying beside her mother, Juli felt as though “there was still a thread of something there.”
On Jan. 20, 2021, a judge granted Kris and Juli guardianship of their mother. Four days later, as the sisters were planning a trip to Omaha, Diane died.
The official cause, listed on her death certificate, was Alzheimer’s disease, but Diane had recently been diagnosed with Covid.
Juli is still holding on to her mother’s ashes, two years later. The sisters don’t want to bury them, in the family plot in Denison, until Denzil dies, because they don’t want him to have a gravesite to visit.
Denzil wonders what will become of Diane’s ashes and whether they will end up in the family plot after all. He wishes that his granddaughter Hayley could have saved him a handful.
Only Hayley was with Diane at the end: sitting at her grandmother’s side, singing whatever songs came to mind, until Diane’s breathing got heavy and stopped.
Hayley didn’t know if Diane knew that she was there, but she seemed to know that someone was with her. “She grabbed my hand,” Hayley said. “She wanted her hand to be held.”
Opening photographs: Diane Norelius with Kris around 1998; Diane with Denzil Nelson around 2015.
Katie Engelhart is a contributing writer for the magazine, focused on ethics and medicine. She is the author of “The Inevitable: Dispatches on the Right to Die,” from St. Martin’s Press.
She won the 2020 George Polk Award for magazine reporting for her investigation into the private nursing-home industry. McNair Evans is a photographer in San Francisco. His work is being exhibited at Tracey Morgan Gallery in Asheville, N.C., in June.